既往有研究发现维生素D水平对肿瘤发生发展有一定的影响,但是并没有具体的结论。维生素D水平是否与癌症患者生存相关?是否补充维生素D能作为预防肿瘤的手段?近期发表的两项研究分别给出了答案。
研究一:癌症诊断时血液维生素D水平较高与明显较好的生存期和缓解率相关
研究人员发现,癌症诊断时血液维生素D水平较高与明显较好的生存期和缓解率相关。这一结果来自于一项涉及17,000例以上癌症患者的综合荟萃分析。
各个瘤种中25(OH)D水平对生存的影响
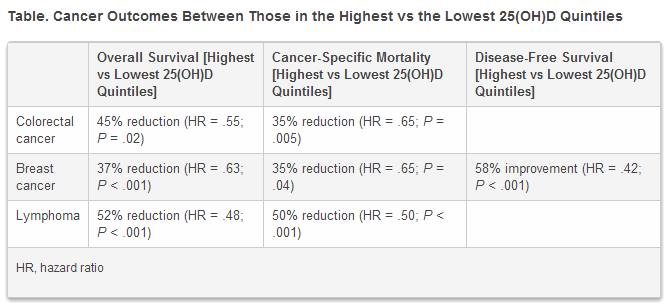
研究者们发现,血液中25-羟基维生素D[25(OH)D]处于较高水平的结直肠癌和乳腺癌患者的总生存期显著优于那些25(OH)D水平处于较低水平的患者。与最低四分之一的患者相比,25(OH)D最高四分之一中的淋巴瘤患者的总生存期显著更好。
各个瘤种中25(OH)D水平对生存的影响
血液中维生素D水平较高明显与结直肠癌和淋巴瘤患者的癌症特异性死亡率较低相关,乳腺癌患者及淋巴瘤患者的无病生存率也有明显改善。
该研究通讯作者,我国上海生命科学研究院营养科学的王慧教授表示:“这项研究可以被认为是支持血液中25(OH)D水平与癌症预后存在相关的最有力的证据,考虑到维生素D缺乏在世界范围内普遍存在,我们的建议是要确保每个人的这种重要的营养素处于足够高的水平,也就是说,血液中的25(OH)D水平在75 nmol/L以上。”
在这项荟萃分析中,作者对25项研究,共17,732例癌症患者进行了研究。来自结直肠癌,乳腺癌和淋巴瘤的证据都强烈支持诊断时血液中高水平25(OH)D具有保护作用。研究人员还在肺癌,胃癌,前列腺癌,白血病,黑色素瘤和Merkel细胞癌患者身上观察到,高水平25(OH)D水平具有保护作用的证据,证据虽然有限但很有利。
事实上,当研究人员对40-70nmol/L与<19nmol/L的25(OH)D进行比较后,他们发现,所有癌症患者(这些患者均进行了剂量-反应关系评估)诊断时血液中维生素D水平每升高10nmol/L,则全因死亡率下降4%。
正如王教授所说,研究人员倾向于认为维生素D是一种癌症化学性预防药物。“很多实验室研究表明,维生素D可能通过作用于肿瘤细胞和调节肿瘤微环境来抑制癌症的进展,此外,维生素D对骨骼健康和免疫系统的生物学作用可能有助于癌症患者较容易挺过艰难的治疗方案,并有助于减轻不良反应。
研究二:缺乏维生素D与欧裔美国男性和非裔美国男性的侵袭性前列腺癌相关
发表在临床癌症研究的另一项研究称,缺乏维生素D与欧裔美国男性和非裔美国男性的侵袭性前列腺癌相关。这些男性患者因列腺特异抗原(PSA)或直肠指检(DRE)异常而进行首次活检。全文下载:Clin Cancer Res.2014 May1;20(9):2289-99
结果表明,25(OH)D水平<12 ng/mL与两组男性较高的Gleason分级(≥4+4)和较高的临床分期(肿瘤分期≥cT2b)呈正相关,但非裔美国男性更具侵略性前列腺癌和缺乏维生素D之间的相关性较强。
根据美国国家综合癌症网络(NCCN)标准,这项研究还发现25(OH)D低水平与较高的前列腺癌风险之间存在相关。
“在我们的研究中,缺乏维生素D似乎是欧裔美国男性和非裔美国男性前列腺癌诊断的预测因子 ”芝加哥西北大学范伯格医学院泌尿外科副教授,第一作者Adam B. Murphy博士在在一份声明中评论说。
Murphy博士补充说:“非裔美国人(更具侵略性前列腺癌和缺乏维生素D)强相关意味着缺乏维生素D在非裔美国男性前列腺癌发病中作用较大(与欧裔美国男性相比)。维生素D补充给药可能是预防前列腺癌发病率和/或前列腺癌患者肿瘤进展的相关策略。”
Review: The Impacts of Circulating 25-Hydroxyvitamin D Levels on Cancer Patient Outcomes: A Systematic Review and Meta-Analysis
Context: Circulating levels of 25-hydroxyvitamin D [25(OH)D] may affect the prognosis of cancer patients; however, the epidemiological results are not consistent.
Objective: To perform a meta-analysis of all published studies to assess the associations of circulating 25(OH)D levels measured at or near the time of diagnosis and outcomes for cancer patients.
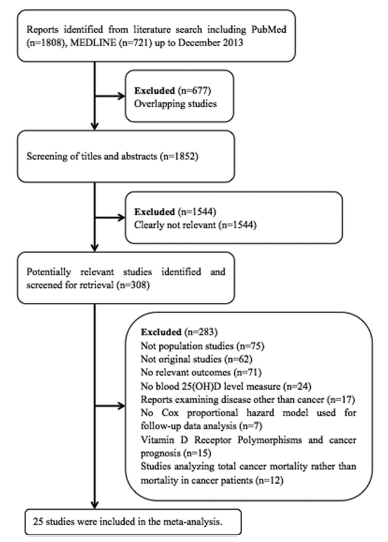
Data Sources: Searches of the PubMed and MEDLINE databases were performed and updated to December 2013.
Study Selection: Studies reporting an association between circulating 25(OH)D levels at or near the time of diagnosis and outcomes for the patients were included.
Data Extraction: Data extraction was performed independently by two authors, and conflicts were resolved by a third investigator.
Data Synthesis: Included in the meta-analysis were 25 studies with 17 332 cases. Significant associations between circulating 25(OH)D levels at or near the time of diagnosis and the outcomes for cancer patients were found. The pooled hazard ratio for the highest vs the lowest quartile of circulating 25(OH)D levels was 0.55 (95% confidence interval [CI] = 0.33–0.91) for overall survival of colorectal cancer patients, 0.63 (95% CI = 0.51–0.77) for breast cancer patients, and 0.48 (95% CI = 0.36–0.64) for lymphoma patients. Higher 25(OH)D levels were significantly associated with reduced cancer-specific mortality for patients with colorectal cancer (P = .005) and lymphoma (P < .001) and improved disease-free survival for patients with breast cancer (P < .001) or lymphoma (P < .05). A 10-nmol/L increment in circulating 25(OH)D levels conferred a hazard ratio of 0.96 (95% CI = 0.95–0.97) for overall survival of the cancer patients.
Conclusions: The results indicate that cancer patients with higher circulating 25(OH)D levels at or near the time of diagnosis have better outcomes.
Affiliations: Key Laboratory of Food Safety Research (M.L., P.C., J.L., R.C., D.X., H.W.), Institute for Nutritional Sciences, Shanghai Institutes for Biological Sciences, Chinese Academy of Sciences, University of the Chinese Academy of Sciences, Shanghai 200031, China; Key Laboratory of Food Safety Risk Assessment (D.X., H.W.), Ministry of Health, Beijing 100021, China; and School of Life Science and Technology (D.X., H.W.), Shanghai Tech University, Shanghai, 200031, China
Vitamin D Deficiency Predicts Prostate Biopsy Outcomes
Purpose: The association between vitamin D and prostate biopsy outcomes has not been evaluated. We examine serum vitamin D levels with prostate biopsy results in men with an abnormal prostate-specific antigen and/or digital rectal examination.
Experimental Design: Serum 25-hydroxyvitamin D (25-OH D) was obtained from 667 men, ages 40 to 79 years, prospectively enrolled from Chicago urology clinics undergoing first prostate biopsy. Logistic regression was used to evaluate the associations between 25-OH D status and incident prostate cancer, Gleason score, and tumor stage.
Results: Among European American (EA) men, there was an association of 25-OH D <12 ng/mL with higher Gleason score ≥ 4+4 [OR, 3.66; 95% confidence interval (CI), 1.41–9.50; P = 0.008] and tumor stage [stage ≥ cT2b vs. ≤ cT2a, OR, 2.42 (1.14–5.10); P = 0.008]. In African American (AA) men, we find increased odds of prostate cancer diagnosis on biopsy with 25-OH D < 20 ng/mL [OR, 2.43 (1.20–4.94); P = 0.01]. AA men demonstrated an association between 25-OH D < 12 ng/mL and Gleason ≥ 4+4 [OR, 4.89 (1.59–15.07); P = 0.006]. There was an association with tumor stage ≥ cT2b vs. ≤ cT2a [OR, 4.22 (1.52–11.74); P = 0.003].
Conclusions: In AA men, vitamin D deficiency was associated with increased odds of prostate cancer diagnosis on biopsy. In both EA and AA men, severe deficiency was positively associated with higher Gleason grade and tumor stage. Clin Cancer Res; 20(9); 2289–99. ©2014 AACR.